Trends and Determinants of Malnutrition in Children-A Sub-Analysis of Pakistan DHS Data
Abrar-ul-Haq Satti1, Muhammad Arsalan Farooq2, Saleha Ahsan3, Muqadar Shah4, Muhammad Imran5, Saira Mehmood6, Raza Hussain Shah7, Maria Shamsher8, Rizwan Taj9, Najma Ayub10, Atteaya Zaman11, Arham Rizwan Khan12 and Saleem Abbasi13*
1Department of Pediatrics, Rawal Institute of Health Sciences, Islamabad, Pakistan
2Department of Pediatrics, Shifa College of Medicine, Shifa International Hospital, Islamabad, Pakistan
3Department of Management, Preston University, Islamabad, Pakistan
4Department of Pediatrics, The Children Hospital, PIMS, Islamabad, Pakistan
5Department of Pediatrics, Shifa International Hospital, Islamabad, Pakistan
6Department of Obstetrics and Gynecology , Rawal Institiute of Health Sciences, Islamabad, Pakistan
7Department of Pediatrics, Ayub Teaching Hospital, MTI, Abbottabad, Pakistan
8Department of Pediatrics, Benazir Bhutto Hospital, Rawalpindi, Pakistan
9Department of Psychiatry, Pakistan Institute of Medical Sciences, Islamabad, Pakistan
10Department of Obstetrics & Gynaecology, HBS Medical and Dental College, Islamabad, Pakistan
11Department of Biochemistry, Federal Medical and Dental College, Shaheed Zul iqar Ali Bhutto Medical University, Islamabad, Pakistan
12Department of Medicine, Shifa College of Medicine, Shifa Internatonal Hospital, Islamabad, Pakistan
13Department of Epidemiology, Pakistan Institute of Medical Sciences, Islamabad, Pakistan
- *Corresponding Author:
- Saleem Abbasi
Department of Epidemiology,
Pakistan Institute of Medical Sciences, Islamabad,
Pakistan
E-mail: saleemsw@hotmail.com
Received date: January 09, 2023, Manuscript No. IPJCND-23-15618; Editor assigned date: January 11, 2023, PreQC No. IPJCND-23-15618 (PQ); Reviewed date: January 25, 2023, QC No. IPJCND-23-15618; Revised date: February 01, 2023, Manuscript No. IPJCND-23-15618 (R); Published date: February 10, 2023, DOI: 10.36648/2472-1921.9.1.184
Citation: Satti AUH, Farooq MA, Ahs an S, Shah M, Imran M, et al. (20 23) Trends and Determinants of Malnutrition in Children-A Sub-Analysis of Pakistan DHS Data. J Clin Nutr Diet Vol.9 No.1:184.
Abstract
Context: Child malnutrition is a serious public health threat. In Pakistan, there is rare data regarding comparison of linear trends and determinants of historical data with recent one.
Objectives: To measure linear trends of child malnutrition and its determinants according to the Pakistan Demographic Health Survey 2017-2018 data.Objectives: To measure linear trends of child malnutrition and its determinants according to the Pakistan Demographic Health Survey 2017-2018 data.
Methods: A sub-analysis of Pakistan DHS data 2017-2018 was conducted and data on 4226 children under 5 years was analyzed. The study outcome was measurement of linear trends of malnutrition over the years from DHS 1991 to up to DHS 2018. Comparison of trends of stunting, wasting and underweight was done between two time periods i.e., 1991 to 2012 (past) and 2013 to 2018 (recent). Analysis was done in STATA 10.0.
Results: The mean age was 2.1 ± 1.3 years with male dominance 2145 (50.7%). Stunting, wasting and underweight rates were measured at 38%, 7.1% and 23.0% respectively. The reduction in stunting and underweight rates was 5% and 10% between 1991 and 2012 whereas wasting increased by 1.6%. In recent past (2013 to 2018) stunting and underweight reduced by 7% points each while wasting dropped by 4%. Chronic malnutrition decreased greatly in the last decade. Lack of paternal education, small size at birth, poor socioeconomic status, home delivery, rural residence, and regions of Sindh and Baluchistan were more likely to suffer from stunting and underweight.
Conclusion: Stunting, wasting and underweight have gained a steady dip recently in Pakistan which is a sign of human and national progress. However, this progress needs sustainability.
Keywords
Children; Determinants; Linear trends; Stunting; Underweight; Wasting
Introduction
Malnutrition, particularly under nutrition continues to be one of the leading causes of morbidity and mortality in children under five whereby around 45% of children die each year globally due to this condition [1,2]. Stunting, wasting, underweight, and micronutrient deficiencies are among the various forms of under nutrition in children <5 years of age which continue to pose a substantial public health problem [3]. Within these five years, the first 2 years of life encompass the critical developmental period which means that early nutritional deficiencies are linked to impaired intellectual performance, reduced work capacity, poor reproductive outcomes and overall poor health during adolescence and adulthood [1,3]. Malnourished children aged less than 5 years are more prone to repeated infections as their low immunity and repeated episodes of infection like diarrhea, pneumonia and other infectious diseases increase risk of severe morbidity and mortality [4]. In the long run, under nutrition hits the economy of a country thus pushing it further into poverty [5].
The highest prevalence of under nutrition is in Lower Middle Income Countries (LMICs) [1]. The trends of under nutrition are variable in the South Asian region, with Pakistan and India being the most affected countries having stunting and underweight rates in the range of 40%-50% and 30%-40% respectively [6]. Unfortunately, these rates have remained high with nonsignificant signs of improvement in the last two decades. On the other hand, demographically and economically similar countries like Bangladesh and Sri Lanka have achieved significant improvement in child malnutrition in recent years [7]. Pakistan is the sixth largest population in the world with an exceptionally high level of child under nutrition. According to Pakistan DHS 2012, stunting rate (45%) ranks at 124 out of 132 countries. Similarly, its wasting rate (11%), ranks 106 out of 130 countries [8]. It is estimated that the outcomes due to under nutrition result in an estimated total economic cost of approximately Rs. 704.3 billion to Pakistan [5]. It is therefore, evident that unless under nutrition is not tackled, it can contribute to massive implications in the future which can drag the country further into poverty.
World Health Organization and UNICEF have emphasized on development of effective and innovative strategies to improve child health in general and under nutrition in particular. However, for those strategies to be developed, high-quality evidence needs to be available that can guide the development of these strategies for policymakers and program managers. In Pakistan, there is limited high quality data available on determining linear trends on under nutrition and therefore, we aim to generate that evidence to inform key stakeholders to transform it into action.
Material and Methods
Data source and ethical considerations
Data for this study came from the Pakistan Demographic and Health Surveys (PDHS) 2017-2018. The DHS data is available in public domain for access (www.measuredhs.com). We downloaded data from Demographic Health Survey (DHS) program after getting permission for sub-analysis. DHS is a nationally representative cross-sectional survey administered by National Institute of Population Studies (NIPS) in collaboration with DHS program with funding from USAID [9]. These surveys have been conducted at varying intervals since 1991 and are still ongoing. The surveys are designed to collect nationally representative data of women of reproductive age and their children and households on their health and welfare. In this survey, as the consent and ethical approval was taken by NIPS and John Snow Inc. at the point of conducting survey, so here in this sub-analysis no consent was taken.
Sampling plan
The PDHS used a multi-staged stratified sampling design whereby Pakistan was divided into regions, which are political regions such as states or provinces. Within the provinces, populations were stratified by urban and rural area of residence. Among these stratified urban and rural areas, a random selection of survey areas was taken from the most recent population census. These Primary Sampling Units (PSUs) were selected based on probability proportional to the population size. In the second stage of sampling, all households were listed within a cluster and randomly selected for an interview by equal-probability systematic sampling. Within each sampled household, the household members were listed and women eligible for a more detailed interview were identified. Usually, the respondent was a woman between 15 and 49 years age.
There were 15671 households surveyed in DHS 2017-2018. Women between 15-49 years were the main respondents who were separately interviewed from Pakistan, Azad Jammu and Kashmir and Gilgit-Baltistan areas. The response rate was 11869/12,338 households yielding a rate of 96% in Pakistan. Similarly, the household response rates were 98% in Azad Jammu and Kashmir and 99% in Gilgit-Baltistan. In the interviewed households, 94% of ever-married women age 15-49 in Pakistan, 97% in Azad Jammu and Kashmir, and 94% in Gilgit- Baltistan were interviewed. The data was assessed for completeness and only cases with complete entries regarding malnutrition parameters of stunting, wasting and underweight were included in the study. We excluded the cases with incomplete information, child not living with mothers, flagged cases and cases with missing values. The complete data on 4226 children under 5 years of age regarding malnutrition was, therefore, analyzed.
Statistical analysis
STATA 10.0 software was used for data analysis. Frequency and percentages were calculated for stunting, wasting and underweight. The indicators of malnutrition were dichotomized on the basis of presence or absence of the condition and were associated with the individual, household and community level factors. The individual level variables included maternal age, maternal education, father’s education, child gender, child age, place of delivery, birth order, preceding birth interval and cesarean delivery. The household level variable included socioeconomic status whereas the community level variables included residence and geographical region. χ2 test was used to associate the trends of stunting, wasting and underweight individually with selective study factors. A significance level of <0.05 was considered statistically significant. Logistic regression analysis was done to find out final predictors of malnutrition. This was unweighted data, so unadjusted OR with 95% confidence intervals were measured. Outcome variables were dichotomized and response of interest was coded as ‘1’ and non-interest as ‘0’. Some of the study indicators were categorized and recoded for this analysis.
Results
In this sub-analysis the trends of child malnutrition (stunting, wasting and underweight) were assessed. There were 4226 children whose malnutrition information was available in DHS data 2017-2018. The mean age was 2.1 ± 1.3 years. There was slight male dominance with 2145 (50.7%) proportion compared to 2081 (49.2%) females.
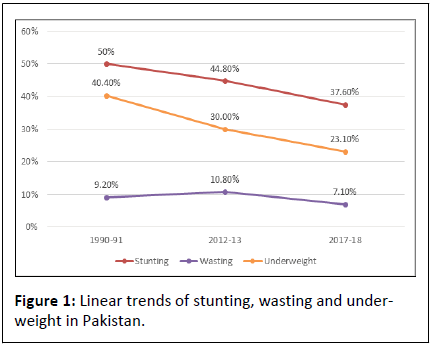
The rates of malnutrition were compared between past and recent years. Between 1990 and 2012 (past) the rates of malnutrition dropped at a slow pace, stunting from 50.0% to 44.8%, underweight from 40.4% to 30.0% whereas wasting inflated from 9.2% to 10.8%. There was a steady drop in malnutrition rates noted between 2013 and 2018 (recent), where stunting dropped from 44.8% to 37.6%, wasting from 10.8% to 7.1% and underweight decreased from 30.0% to 23.1%. When compared between 1990 to 2012 and 2013-2018, stunting decreased 5% previously compared to 7% in the recent times. Wasting inflated 2% in the past compared to a 4%decrease recently, the rate of underweight dropped 10%. The rate of decrease in the malnutrition indicators was similar across the two time periods despite the fact that the former was two decades period (1990-2012) whereas the later was only one decade period (2013-2018) (Table 1) and (Figure 1).
| DHS 1990-91 | DHS 2012-13 | DHS 2017-18 | |
|---|---|---|---|
| Stunting | 2018/4037 (50.0%) | 1553/3466 (44.8%)1 | 1588/4226 (37.6%)2 |
| Wasting | 371/4037 (9.2%) | 374/3466 (10.8%) | 304/4226 (7.1%)3 |
| Underweight | 1631/4037 (40.4%) | 1040/3466 (30.0%)4 | 984/4226 (23.1%)5 |
Note: Highly significant differences; 1. 1990-91 and 2012-13: chi squared value 20.257; p-value <0.001, 2. 2012-13 and 2017-18: chi squared value 41.182; p-value <0.001, 3. 2012-13 and 2017-18: chi squared value 30.653; p-value <0.001, 4. 1990-91 and 2012-13: chi squared value 87.605; p-value <0.001, 5. 2012-13 and 2017-18: chi squared value 44.368; p-value <0.001.
Table 1: Comparison of rates of stunting, wasting and underweight between different PDHS.
We also assessed the determinants of stunting, wasting and underweight on the basis of DHS 2017-2018 data. Univariate analysis found out that stunting rates were significantly high in children of uneducated mothers than those having secondary or above education (46.7% versus 23.3%, p-value <0.001). Similarly, non-education status was related to high wasting and underweight rates. Similar trend was witnessed in father’s education. Furthermore, home delivery vs health facility delivery (45.3% versus 33.0%) and cesarean section versus non-cesarean delivery (40.0% versus 25.3%) were also found related with higher rates of stunting and it was also found related to wasting and underweight (p-value, <0.001). Child age of 1 year or above, small size at birth was found having significantly higher malnutrition parameters. Poor socioeconomic status and children from regions of Sindh, KPK, Balochistan and Gilgit- Baltistan were also found to have high rates of stunting and underweight (p-value, <0.001). Rural residence was related to high rates of stunting and underweight (p-value, <0.001). There was no difference in the rates of stunting, wasting and underweight according to maternal age and child sex. Moreover, no difference in the rates of wasting was observed according to child residence, birth order and birth interval (Table 2).
| Height-for-age | Weight-for-age | Weight-for-height | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Stunted (n=1580) | Normal (n=2646) | p-value | Wasted (n=334) | Normal (n=3892) | p-value | Underweight (n=984) | Normal (n=3289) | p-value | |
| Individual level factors | - | - | - | - | - | - | - | - | - |
| Maternal age (years) | - | - | - | - | - | - | - | - | - |
| Up to 20 | 88 (37.7%) | 145 (62.3%) | 0.38 | 26 (11.1%) | 207 (88.8%) | 0.151 | 65 (27.3%) | 173 (72.6%) | 0.15 |
| 21 to 30 | 926 (38.2%) | 1497 (61.7%) | 190 (7.8%) | 2234 (92.1%) | - | 543 (22.1%) | 1905 (77.8%) | - | |
| 31 or above | 566 (36.0%) | 1004 (63.9%) | 118 (7.5%) | 1451 (92.4%) | - | 376 (23.6%) | 1211 (76.3%) | - | |
| Maternal education | - | - | - | - | - | - | - | - | - |
| No education | 1016 (46.7%) | 1159 (53.2%) | <0.001 | 215 (9.8%) | 1959 (90.1%) | <0.001 | 687 (31.2%) | 1511 (68.7%) | <0.001 |
| Primary | 208 (35.9%) | 371 (64.0%) | 34 (5.8%) | 545(94.1%) | 118 (20.1%) | 467 (79.8%) | |||
| Secondary or above | 356 (23.3%) | 1116 (76.7%) | 85 (5.7%) | 1388 (94.3%) | 179 (11.5%) | 1311 (88.4%) | |||
| Father’s education | - | - | - | - | - | - | - | - | - |
| No education | 559 (48.3%) | 598 (51.6%) | <0.001 | 119 (10.2%) | 1037 (89.7%) | <0.001 | 406 (34.7%) | 761 (65.2%) | <0.001 |
| Primary | 265 (42.7%) | 355 (57.2%) | 41 (6.5%) | 581(93.4%) | 148 (23.6%) | 479 (76.4%) | |||
| Secondary or above | 742 (30.4%) | 1650 (69.6%) | 170 (7.5%) | 2221 (92.5%) | 421 (16.8%) | 2001 (82.7%) | |||
| Place of delivery | - | - | - | - | - | - | - | - | - |
| Home | 671 (45.3%) | 808 (54.6%) | <0.001 | 157 (10.6%) | 1324 (89.4%) | <0.001 | 493 (33.0%) | 998 (66.9%) | <0.001 |
| Health facility | 909 (33.0%) | 1838 (66.9%) | 177 (6.4%) | 2568 (93.5%) | 491 (17.6%) | 2291 (82.3%) | |||
| Delivery by cesarean | - | - | - | - | - | - | - | - | - |
| Yes | 186 (25.3%) | 549 (74.6%) | <0.001 | 36 (4.9%) | 171 (7.9%) | 0.001 | 93 (12.4%) | 653 (87.5%) | <0.001 |
| No | 1394 (40.0%) | 2091 (60.0%) | 295 (8.4%) | 3191 (91.5%) | 890 (25.2%) | 2631 (74.7%) | |||
| Child sex | - | - | - | - | - | - | - | - | - |
| Male | 815 (38.0%) | 1330 (62.0%) | 0.41 | 171 (7.9%) | 1974 (92%) | 0.872 | 512 (23.5%) | 1658 (76.4%) | 0.37 |
| Female | 765 (36.7%) | 1316 (63.2%) | 163 (7.8%) | 1918 (92.1%) | 472 (22.4%) | 1631 (77.5%) | |||
| Child age (mon) | - | - | - | - | - | - | - | - | - |
| Up to 6 | 85 (19.8%) | 344 (80.1%) | <0.001 | 48 (11.1%) | 382 (88.8%) | <0.001 | 85 (19.5%) | 351 (80.05%) | <0.001 |
| 6 to 11 | 71 (18.0%) | 323 (81.9%) | 63 (15.9%) | 331 (84%) | 74 (18.6%) | 323 (81.3%) | |||
| 12 to 17 | 133 (27.6%) | 348 (72.3%) | 38 (7.9%) | 443 (92.1%) | 283 (76.6%) | 422 (86.1%) | |||
| 18 to 23 | 153 (42.1%) | 210 (57.8%) | 30 (8.2%) | 333 (91.7%) | 86 (23.3%) | 283 (76.6%) | |||
| 24 to 35 | 372 (44.4%) | 465 (55.5%) | 57 (6.8%) | 780 (93.1%) | 217 (25.4%) | 635 (74.5%) | |||
| 36 to 59 | 752 (44.3%) | 942 (55.6%) | 97 (5.7%) | 1596 (94.2%) | 445 (26.1%) | 1256 (73.8%) | |||
| Size of baby at birth | - | - | - | - | - | - | - | - | - |
| Large | 91 (28.7%) | 226 (71.2%) | <0.001 | 7 (2.2%) | 310 (97.7%) | <0.001 | 38 (11.8%) | 283 (88.1%) | <0.001 |
| Average | 1160 (36.4%) | 2023 (63.5%) | 255 (8%) | 2928 (91.9%) | 712 (22.1%) | 2508 (77.8%) | |||
| Small | 397 (45.3%) | 397 (54.6%) | 654 (90%) | 72 (9.9%) | 234 (31.9%) | 498 (68.0%) | |||
| Birth order | - | - | - | - | - | - | - | - | - |
| 1 | 352 (33.6%) | 694 (66.3%) | <0.001 | 72 (6.8%) | 975 (93.1%) | 0.313 | 209 (19.6%) | 855 (80.3%) | <0.001 |
| 2-4 | 788 (36.8%) | 1349 (63.1%) | 175 (8.05%) | 1964 (91.9%) | 470 (21.7%) | 1689 (78.2%) | |||
| 5 or above | 440 (42.1%) | 603 (57.8%) | 90 (8.6%) | 953 (91.3%) | 305 (29.05%) | 745 (70.9%) | |||
| Birth interval (months) | - | - | - | - | - | - | - | - | - |
| No previous birth | 352 (33.6%) | 694 (66.3%) | <0.001 | 72 (6.8%) | 975 (93.1%) | 0.065 | 209 (19.6%) | 855 (80.3%) | 0 |
| 9 to 14 | 106 (42.2%) | 145 (57.7%) | 18 (7.1%) | 233 (92.8%) | 75 (29.5%) | 179 (70.4%) | |||
| 14 to 24 | 368 (42.4%) | 498 (57.5%) | 57 (6.5%) | 808 (93.4%) | 226 (25.8%) | 648 (74.1%) | |||
| 25 or above | 749 (36.4%) | 1306 (63.5%) | 186 (9.0%) | 1869 (90.9%) | 470 (22.6%) | 1603 (77.3%) | |||
| Household level factors | - | - | - | - | - | - | - | - | - |
| Socio economic status | - | - | - | - | - | - | - | - | - |
| Poor | 935 (48.4%) | 1021 (51.5%) | <0.001 | 199 (10.1%) | 1756 (88.9%) | <0.001 | 644 (34.0%) | 1322 (66.1%) | <0.001 |
| Middle | 282 (35.0%) | 523 (64.9%) | 53 (6.5%) | 753 (93.4%) | 148 (18.1%) | 670 (81.9%) | |||
| Rich | 363 (24.7%) | 1102 (75.3%) | 82 (5.5%) | 1383 (94.4%) | 191 (12.2%) | 1297 (87.8%) | |||
| Community level factors | - | - | - | - | - | - | - | - | - |
| Residence | - | - | - | - | - | - | - | - | - |
| Urban | 625 (32.4%) | 1301 (67.5%) | <0.001 | 158 (8.2%) | 1766 (91.7%) | 0.502 | 379 (19.4%) | 1570 (80.5%) | <0.001 |
| Rural | 955 (41.5%) | 1345 (58.4%) | 176 (7.6%) | 2126 (92.3%) | 605 (26.03%) | 1719 (73.9%) | |||
| Geographical region | - | - | - | - | - | - | - | - | - |
| Punjab | 270 (29.8%) | 636 (70.2%) | <0.001 | 38 (4.2%) | 867 (95.8%) | <0.001 | 132 (14.4%) | 782 (85.5%) | <0.001 |
| Sindh | 362 (44.9%) | 444 (55.0%) | 81 (10.5%) | 725 (89.9%) | 290 (35.4%) | 528 (64.5%) | |||
| KPK | 423 (42.6%) | 630 (57.3%) | 75 (7.2%) | 979 (92.8%) | 225 (21.5%) | 838 (78.4%) | |||
| Balochistan | 239 (46.5%) | 274 (53.4%) | 101 (19.6%) | 412 (80.3%) | 218 (42.0%) | 301 (58.0%) | |||
| Gilgit Baltistan | 109 (39.2%) | 169 (60.7%) | 3 (1.08%) | 275 (98.9%) | 35 (12.5%) | 244 (87.4%) | |||
| Islamabad (ICT) | 48 (22.3%) | 167 (77.6%) | 10 (4.2%) | 224 (95.7%) | 22 (9.1%) | 218 (90.8%) | |||
| AJK | 121 (27.7%) | 315 (72.2%) | 26 (5.9%) | 410 (94.04%) | 62 (14.0%) | 378 (85.9%) | |||
Table 2: Distribution of rates of determinants of stunting, wasting and underweight according to PDHS 2017-2018.
Further analysis was done to find out the final determinants of malnutrition. Results of the logistic regression model revealed that matriculation or higher maternal education (OR (95% CI); pvalue, 0.60 (0.56-0.65); <0.001) and father education (OR (95% CI); p-value, 0.66 (0.61-0.71); <0.001) were less likely to have stunting. Higher education was also found lefiguss likely to have wasting and underweight status. Similarly, healthcare facility delivery (OR (95% CI); p-value, 0.59 (0.52-0.67); <0.001) and cesarean delivery (OR (95% CI); p-value, 0.51 (0.42-0.60); <0.001) were found to have less chance of stunting and a similar trend was noted of these determinants towards wasting and underweight. Furthermore, child age above 1 year (OR (95% CI); p-value, 1.29 (1.24-1.34); <0.001), small size at birth (OR (95% CI); p-value, 1.43 (1.26-1.63); <0.001), birth order of 5 or above (OR (95% CI); p-value, 1.21 (1.09-1.31); <0.001) and rural residence (OR (95% CI); p-value, 1.47 (1.30-1.67); <0.001) were found more likely to be associated with stunting and also with underweight status. Middle or rich socio-economic status (OR (95% CI); p-value, 0.59 (0.55-0.64); <0.001) and geographical regions of Punjab, GB, AJK and ICT (OR (95% CI); p-value, 0.96 (0.93-0.99); <0.001) were less likely to have stunting (Table 3).
| Stunting | Wasting | Underweight | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Secondary or above maternal education | 0.6 | 0.56-0.65 | <0.001 | 0.73 | 0.64-0.83 | <0.001 | 0.54 | 0.50-0.59 | <0.001 |
| Secondary or above father’s education | 0.66 | 0.61-0.71 | <0.001 | 0.71 | 0.6-0.81 | <0.001 | 0.59 | 0.54-0.65 | <0.001 |
| Health facility delivery | 0.59 | 0.52-0.67 | <0.001 | 0.58 | 0.46-0.72 | <0.001 | 0.43 | 0.37-0.50 | <0.001 |
| Cesarean delivery | 0.51 | 0.42-0.60 | <0.001 | 0.55 | 0.39-0.79 | <0.001 | 0.42 | 0.33-0.52 | <0.001 |
| Child age of above 1 year | 1.29 | 1.24-1.34 | <0.001 | 0.82 | 0.78-0.88 | <0.001 | 1.12 | 1.07-1.17 | <0.001 |
| Small baby at birth | 1.43 | 1.26-1.63 | <0.001 | 1.55 | 1.23-1.94 | <0.001 | 1.75 | 1.51-2.03 | <0.001 |
| Birth order of 5 or above | 1.21 | 1.09-1.31 | <0.001 | - | - | - | 1.27 | 1.17-1.44 | <0.001 |
| Middle and/or Rich socioeconomic status | 0.59 | 0.55-0.64 | <0.001 | 0.71 | 0.62-0.81 | <0.001 | 0.53 | 0.49-0.58 | <0.001 |
| Rural residence | 1.47 | 1.30- 1.67 | <0.001 | - | - | - | 1.45 | 1.26-1.68 | <0.001 |
| Geographical regions of Punjab, GB, ICT and AJK | 0.96 | 0.93- 0.99 | 0.032 | - | - | - | 0.94 | 0.90-0.97 | 0.002 |
Table 3: Final determinants of stunting, wasting and underweight based on logistic regression analysis (PDHS 2017-18).
Discussion
The current study highlighted country level spread of malnutrition over the years and its significant determinants. Child malnutrition in Pakistan was compared between two time periods in the last 3 decades, first period between 1990 and 2012 (past) and the second between 2012 and 2018 (recent). The overall trends of malnutrition parameters are on a sliding slope, however, the drop witnessed between almost 22 years period i.e., 1990 to 2012 has been found almost same to that of 5-6 years period between 2012 and 2018. This fact has been studied in the recent past and it was proven that in the two decades between 1990 to 2012 merely 5% reduction, a snail pace in stunting has been achieved [10]. A study by Krishna, et al. reported that the pace of annual reduction in stunting rates was three-to-four times greater in Nepal and Bangladesh when compared to Pakistan and India. They witnessed that in South Asian region between 1991 to 2014, Bangladesh and Nepal recorded the highest reduction in stunting rates annually 2.9 and 4.1 percentage points, compared to 1.3 and a merely 0.6 percentage points in India and Pakistan, respectively [11]. The reduction in stunting quantified currently has programmatic implications and becomes more crucial as between 2013 to 2018 a reduction rate of 1.4% points has been witnessed in Pakistan yearly, showing a rapid jump and also bypassing India’s annual reduction rate [12]. The overall rate of stunting is standing at approximately 38% at current in Pakistan still higher than Bangladesh and Nepal only better than Afghanistan in South Asian region posing a huge challenge for healthcare providers and program managers [13,14]. Scientific body of evidence recommends that children with stunting suffer from worse health and poorer developmental outcomes [15,16]. Chronic malnutrition halts pace of human development and subsequently continues a trapped cycle of low output going at personal and community level [17]. Thus, the reduction achieved in stunting by Pakistan recently needs to be continued at same or better pace so that long term individual and national level losses could be curtailed. Targeted interventions can transform these losses to benefits which could gain fruition. Around the globe, Asia and African regions are the worst affected areas by malnutrition; however, Pakistan also lies among the top countries where high rates of stunting, wasting and underweight are present [18].
It is well known that malnutrition is directly proportional to food availability, feeding habits and food security which are all attributable to a country’s political stability, security and economic development [19]. If these arguments are factual there must have been great economic drive and sustainability between the later shorter periods in Pakistan which achieved highly significant drop in the childhood malnutrition parameters. This analysis found out highly significant drop in the rates of stunting, wasting and underweight in Pakistani children, when compared between both the hypothesized time periods the drop was found equivalent, however, there is huge gap in the time periods. This need to be further explored and validated by correlating these findings with economic data at the national level.
The determinants of malnutrition continue to remain the same over the years and further indicators are entering the list. This study proved that lack of paternal education or primary level education was related to stunting, wasting, and underweight and so was home delivery and non-cesarean delivery. This analysis revealed that child age above 1 year was more likely to have stunting and underweight whereas it was less likely to have wasting. Baby’s small size at birth, 5th or above birth order, and rural residence were also found associated with stunting and being underweight. Further, rich socioeconomic status and geographical regions of Punjab, GB, ICT and AJK were less likely to have stunting and underweight status. The regions of Sindh and Balochistan have exceptionally higher chronic malnutrition in the form of stunting and underweight. Many previous studies from the South Asian region and Pakistan have also concluded these associated indicators. A recent local study by Khan, et al also witnessed that rural residence, low maternal education, and small size of the baby at birth were more likely to be malnutrition [20]. A previous subanalysis of DHS 2012-2013 also presented a similarly associated indicators stratum, however, this current study has highlighted some more determinants of wasting as well which were not present in the previous analysis [21]. Saha, et al. also noted that there were geographical variations in the reduction in stunting rates in Bangladesh with most of the change happening in the major metropolitans such as Dhaka, Rajshahi, Khulna, and Chitagong than those living in Sylhet and Barisal [22]. This variation was also witnessed in the present study where Sindh, Balochistan and KPK had high stunting compared to Punjab, GB, AJK, and ICT regions. Geographical area wise within Pakistan, Islamabad remained stagnant at 22%. Punjab, Sindh and GB gained approximately 9%-10% reduction in stunting but the greatest slump was gained by Balochistan where rates dropped from 78% in 2012 to 46% in 2018. With a focused equitable approach, the disparity in stunting rates in different regions can be addressed. Health ministries and programmes, NGOs and other stakeholders could play a vital role in streamlining strategies and interventions to tackle malnutrition in different regions and demographics.
It was witnessed that while comparing stunting rates between continents and larger regions; South Asia takes the lead from all other regions including Africa; this has a direct relation to socioeconomic background of peoples in the region [23]. Heath bodies and international financial institutes must come together and forward to make strategies to get rid of chronic malnutrition in the region.
This analysis has many advantages and implications; firstly, evidence generation is important for countries like Pakistan where malnutrition is still a huge problem [24]. The respective ministries and departments could benefit from these evidences and strategies plans to tackle child malnutrition better. Since, malnutrition is associated with low socioeconomic status the financial departments and institutions planning and executing policies could make equitable strategies keeping in mind the most vulnerable groups and areas in Pakistan.
This was a cross-sectional survey-based data and no follow-up of study cases could be completed which could have in turn shown long term status of these children and their health and developmental outcomes.
Conclusion
The rates of stunting, wasting and underweight have seen a significant dip in the recent decade in Pakistan which is a good sign and a hallmark of speedy health improvement as well as human and national development. However, chronic malnutrition is still high in Pakistan compared to other regional countries. Paternal educational status, socioeconomic class and access to healthcare services continue to haunt program managers and health administrators as they are trending in Pakistan for many decades now. As there was a speedy reduction in stunting, wasting and underweight in the recent times, there is a need to further look in to the causes especially, economic, social and health conditions of local communities.
Funding Source
This study did not receive any financial funding.
Authors Contributor Ship
All the authors participated in the conceptualization and plan of the study. Saleem Abbasi analyzed the data and wrote the results. Abrar-ul-Haq Satti, Muhammad Arsalan Farooq, Saleha Ahsan and Muhammad Imran wrote the introduction and method sections. All the authors contributed in writing the discussion section. The draft manuscript was critically reviewed by Rizwan Taj, Atteaya Zaman and Saleem Abbasi.
Acknowledgement
We acknowledge the DHS program USA portal for providing access to DHS data. We also acknowledge the University of Sydney which provided the license of STATA software and also provided the technical assistance.
Competing Interests
All the authors mentioned that “there is no conflict of interest”.
References
- Ma’alin A, Birhanu D, Melaku S, Tolossa D, Mohammed Y, et al. (2016) Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: A cross-sectional study. BMC Nutrition 2: 44.
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, et al. (2013) Maternal and child under nutrition and overweight in low-income and middle-income countries. The Lancet 382: 427-451.
[Crossref],[Google Scholar],[Indexed]
- Tzioumis E, Kay MC, Bentley ME, Adair LS (2016) Prevalence and trends in the childhood dual burden of malnutrition in low-and middle-income countries, 1990–2012. Public health nutrition 19: 1375-1388.
[Crossref],[Google Scholar],[Indexed]
- Aheto JMK, Keegan TJ, Taylor BM, Diggle PJ (2015) Childhood malnutrition and its determinants among under-five children in Ghana. Matern Child Nutr 29: 552-561.
[Crossref],[Google Scholar],[Indexed]
- https://econpapers.repec.org/paper/fprpacern/2.htm
- Bhutta, ZA, Gazdar H, Haddad L (2013) Seeing the unseen: Breaking the logjam of under nutrition in Pakistan. Ids Bull I Dev Stud 44: 1-9.
- Khan JR, Awan N (2017) A comprehensive analysis on child mortality and its determinants in Bangladesh using frailty models. Arch Public Health 75: 58.
[Crossref],[Google Scholar],[Indexed]
- Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: A cross-sectional study
- http://www.nips.org.pk/abstract_files/ Preliminary Report Final.pdf
- https://econpapers.repec.org/paper/esswpaper/id_3a5060.htm
- Krishna A, Mejía‐Guevara I, McGovern M, Aguayo VM, Subramanian SV (2018) Trends in inequalities in child stunting in South Asia. Matern Child Nutr 14: e12517.
[Crossref],[Google Scholar],[Indexed]
- Avula R, Raykar N, Menon P, Laxminarayan R (2016) Reducing stunting in India: What investments are needed? Matern Child Nutr 12: S249‐S252.
[Crossref],[Google Scholar],[Indexed]
- https://www.un-ilibrary.org/content/periodicals/1564975x
- Akhtar S (2015) Malnutrition in South Asia-A critical reappraisal. Critical Reviews in Food Science and Nutrition 56: 2320-2330.
[Crossref],[Google Scholar],[Indexed]
- Black MM, Walker SP, Fernald L, Anderson CT, DiGirolamo AM, et al. (2016) Early childhood development coming of age: Science through the life course. The Lancet: 1-14.
[Crossref],[Google Scholar],[Indexed]
- Black RE, Alderman H, Bhutta ZA, Gillespie S, Haddad L, et al. (2013) Maternal and child nutrition: Building momentum for impact. The Lancet 382: 372-375.
[Crossref],[Google Scholar],[Indexed]
- Reinhardt K, Fanzo J (2014) Addressing chronic malnutrition through multi-sectoral, sustainable approaches: A review of the causes and consequences. Front Nutr 1: 13.
[Crossref],[Google Scholar],[Indexed]
- Burchi F, Fanzo J, Frison E (2011) The role of food and nutrition system approaches in tackling hidden hunger. Int J Environ Res Public Health 8: 358‐373.
[Crossref],[Google Scholar],[Indexed]
- Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ (2017) Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006-2016). PLoS One 12: e0177338.
[Crossref],[Google Scholar],[Indexed]
- Khan S, Zaheer S, Safdar NF (2019) Determinants of stunting, underweight and wasting among children <5 years of age: Evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health 19: 358.
[Crossref],[Google Scholar],[Indexed]
- Abbasi S, Mahmood H, Zaman A, Farooq B, Malik A, et al. (2018) Indicators of malnutrition in under 5 Pakistani children: A DHS data secondary analysis. J Med Res Health Educ 2: 12.
- Saha UR, Chattapadhayay A, Richardus JH (2019) Trends, prevalence and determinants of childhood chronic under nutrition in regional divisions of Bangladesh: Evidence from demographic health surveys, 2011 and 2014. PLOS One 14: e0220062.
[Crossref],[Google Scholar],[Indexed]
- Gillespie S, VanDen BM, Hodge J, Herforth A (2015) Leveraging agriculture for nutrition in South Asia and East Africa: Examining the enabling environment through stakeholder perceptions. Food Sec 7: 463-477.
- Asim M, Nawaz Y (2018) Child malnutrition in Pakistan: Evidence from literature. Children 5: 60.
[Crossref],[Google Scholar],[Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences