Effect of the Use of Probiotics and High Fiber Diet in Patients with Obesity: A Randomized Clinical Trial
Maria De Lourdes Lima De Souza E Silva* and Renata Oliveira Dos Santos Menezes
Department of Medicine and Human Health, Bahia School of Medicine and Public Health, Salvador, Bahia, Brazil
*Corresponding author:
Renata Oliveira Dos Santos Menezes,
Department of Medicine and Human Health, Bahia School of Medicine and Public Health, Salvador, Bahia, Brazil,E-mail: renata.oliveira.nut@gmail.com
Received date: July 04, 2022, Manuscript No. IPJCND-22-13941; Editor Assigned date: July 07, 2022, PreQC No. IPJCND-22-13941(PQ); Reviewed date: July 18, 2022, QC No. IPJCND-22-13941; Revised date: July 25, 2022, Manuscript No. IPJCND-22-13941(R); Published date: August 10, 2022, DOI: 10.36648/2472-1921.8.7.180
Citation: De-Souza-E-Silva MDLL, Santos-Menezes ROD (2022) Effect of the Use of Probiotics and High Fiber Diet in Patients with Obesity: A Randomized Clinical Trial. J Clin Nutr Diet Vol.8 No.7: 180.
Abstract
Background: This investigation was carried out in order to verify, in a specific sample (women, from the Northeast of Brazil), the effect of probiotics with multiple strains associated or not with a diet rich in fiber with prebiotic action on weight and the metabolic markers investigated in cases of metabolic syndrome, in order to compare what the literature has been describing for more than ten years, based on studies carried out with animals or humans, whose population has never been so selected, in order to be able to safely apply the use of probiotics for the aforementioned purpose in the tested population.
Thus, the objective of this study was to compare the effect of the use of probiotics with multiple strains associated with a diet rich in fiber with prebiotic action and reduced in sugars and fats with the effect of the same diet alone, in the control of dysbiosis, weight and metabolic markers in overweight women.
Introduction: Many animal studies have shown that obesogenic mechanistic pathways can be modulated by probiotics and prebiotics. This study aimed to compare the effect of the use of probiotics with multiple strains associated with a diet rich in fiber with prebiotic action and reduced in sugars and fats for three months, with the effect of the same diet alone, in the control of dysbiosis, weight and of metabolic markers in overweight women.
Methods and Findings: This is a randomized, double-blind, placebo-controlled clinical trial conducted with 72 patients in Salvador, Bahia, Brazil. Patients were divided into two groups and received either probiotic strains or placebo once daily. Both groups received dietary guidelines for increasing fiber. Anthropometric and laboratory assessments were performed before and after the intervention, a questionnaire was applied to screen the risks for dysbiosis and food frequency.
Results: We evaluated 72 low-income women, with a mean age of 55 years. There was adherence to the diet by approximately 39% of the sample. In both groups there was improvement in dysbiosis, significant weight loss in the test group and slight gain in the placebo group. There was an improvement in the lipid profile in both groups, with significance only in the placebo group. There was no change in the glycemic profile. The analysis of the results showed efficiency of probiotics in weight control, probable efficiency of fibers per si and of probiotics in controlling dysbiosis and lipid profile, with no significant difference between GT and GP, as there was an improvement in both, and no better pattern was identified on glycemic control in both groups.
Conclusion: Confounding factors were identified during the development of the research and, therefore, new studies aimed at comparing the effectiveness of the use of probiotics with or without prebiotics in controlling the variables investigated here, aiming to contribute with evidence that is sufficient to recommend the treatment of intestinal dysbiosis, controlling for the possible biases identified here.
Keywords: Dysbiosis; Obesity; Probiotic; Prebiotic; fibers; Weight loss; Lipid profile.
Introduction
Obesity is a complex and multifactorial disease associated with several factors, including host genetics, decreased physical activity and excessive food intake [1]. In recent decades, the gut microbiota has been proposed as an additional factor that favors fat storage, weight gain, and insulin resistance. It inhibits the release of Fasting-Induced Adipose Factor (FIAF), an inhibitor of Lipoprotein Lipase (LPL) activity, resulting in the subsequent storage of triglycerides in adipose tissue and liver, and influences the development of metabolic endotoxemia and low-grade inflammation [2,3]. Which culminates in obesity and its comorbidities the synergy of the high-fat diet and the dysbiotic gut microbiota initiates a recipe that epigenetically programs the host for increased adiposity and poor glycemic control [4].
Thus, dysbiosis, characterized by the imbalance of the intestinal microbiota, with a predominance of more virulent microorganisms, leading to deleterious effects on the health of the host, has been associated with several chronic pathological conditions, such as obesity, type 2 diabetes (DM2), dyslipidemia and atherosclerosis [5,6]. It is related to stress, factors associated with the modern lifestyle, including the consumption of foods low in fiber, pesticides, antibiotics, among others.
The intestinal microbiota is a complex community of microorganisms that inhabit the gastrointestinal tract and establish a close symbiotic relationship with the human host. It plays a crucial role in maintaining health, allowing the metabolism of indigestible food components and the synthesis of some vitamins, preventing the colonization of pathogens and contributing to the maintenance of the immune system [7]. It is mainly composed of two bacterial phyla, Firmicutes and bacteroidetes that represent more than 90% of the total community [3]. Studies show that the predisposition to increase body fat or obesity is determined by the Firmicutes: Bacteroidetes (F:B) ratio [8-10].
Obese microbiota exhibit significantly elevated F:B ratio compared to lean gut microbiota, even when food/energy consumption between groups is similar. Obese individuals show up to 50% less Bacteroidetes and more Firmicutes than lean individuals. On the other hand, the composition of Bacteroidetes in the obese microbiota is increased, while Firmicutes is reduced when there is weight loss and reduced consumption of a high-fat/carbohydrate diet, which shows how diet can influence the characteristic of the microbiota [11,12]. In addition, many studies carried out mostly with animals have shown that, interestingly, these mechanistic obesogenic pathways that are transmissible from one generation to another can be modulated through the administration of probiotics and prebiotics [4].
However, these microbiota changes may not be observed in some cases due to confounding factors that affect the composition of the gut microbiota beyond the dietary content, including fasting, antibiotic use, age, geographic location, intensity and regularity of the diet. Exercise, genetic, technical and clinical factors [13-15].
According to the World Health and Food Organization and the United Nations, probiotics are live microorganisms that, when administered in amounts, confer a health benefit on the host [16]. Human studies have reported improvements in the lipid profile, in particular, decreased level of TC, LDL-c and plasma TG and increased HDL-c, also insulin sensitivity and therefore obesity resulting from hypothalamic control of food intake and insulin signaling [17]. Prebiotics, on the other hand, are defined as non-digestible food ingredients (usually polysaccharides) capable of selectively stimulating the growth and/or activity of the microbiota, especially lactobacilli and bifidobacteria, thus providing health-promoting effects on the energy balance of the host, being able to be fermented by bacteria, giving rise to Short Chain Fatty Acids (SCFA) [18,19].
The objective of this study was to compare the effect of the use of probiotics with multiple strains associated with a diet rich in fiber with prebiotic action and reduced in sugars and fats with the effect of the same diet alone, in the control of dysbiosis, weight and metabolic markers in overweight women.
Materials and Methods
This 12-week, randomized, double-blind, placebo-controlled clinical trial was conducted in a multi-professional public outpatient clinic specializing in the treatment of obesity, in Salvador, Bahia, with 80 patients. The clinical protocol was approved by the Ethics Committee and all included patients gave their written consent before being screened for the study, which was registered in the Brazilian Registry of Clinical Trials (REBEC) under the UTN number: U1111-1220-2109.
Female patients aged over 18 years, Body Mass Index (BMI) greater than or equal to 25 kg/ m² and Waist Circumference (WC) greater than 80 cm, participants of the Project for the study of excess were included [20]. Weight Management System (PEPE), with risk of dysbiosis detected by the DIS questionnaire (prepared by the researchers), by inviting the most assiduous patients from a universe of 250 patients and subsequent randomization. To calculate the sample size, a significance level of 5% and statistical power of 80% were considered for a minimum weight reduction of 500 g per week. The 95% confidence interval was taken into account, according to data from previous studies.
Women whose level of understanding and communication compromised the accuracy of the answers to the applied questionnaires, pregnant or lactating women, patients undergoing chronic hemodialysis, those using estrogens, chemotherapy drugs, anorectics, antibiotics, insulin and anabolic steroids were excluded.
Patients included in the clinical trial were randomly allocated to receive probiotic supplementation (test group-GT), composed of 109 CFU of each of the following strains: Lactobacillus acidophilus, lactobacillus rhamnosus, lactobacillus paracasei and bifdobacterium lactis; or placebo, composed of insoluble fibers (placebo group-GP), packed in identical sachets. The eight-block randomization plan was generated by a professional not involved in any other phase of the research. Both groups received qualitative guidelines for a diet rich in fiber, with foods containing FOS (fructooligosaccharides), with reduced amounts of simple carbohydrates and fats.
The initial assessment took place after screening and acceptance of the invitation, when patients came to the outpatient clinic to sign the informed consent, answer the DIS questionnaire (prepared by the researchers) to assess the risk of dysbiosis (which includes information about lifestyle, age, surgery and/or use of antibiotics and anti-inflammatory drugs in the previous 30-day interval) and to the Qualitative Food Survey (IAQ), to verify eating habits, which is a food frequency questionnaire organized by food groups, and to be sent to the laboratory for blood collection for laboratory tests (fasting glucose, glycated hemoglobin, Total Cholesterol (TC) and fractions, triglycerides, determination of Homa-IR Index (insulin resistance being considered if greater than 4.65 alone or greater than 3 .60 and BMI greater than 27.5 kg/ m2, fecal pH and Dysbiosis Test (INDICAN), which is the result of the decomposition of tryptophan I intestinal tract, being normally present in traces in the urine, identified from the Obermayer reaction [21-23]. According to the results of this examination, if dysbiosis is present, it can be classified as mild (+/ IV or ++/ IV), moderate (++/ IV) or severe (++++/ IV).
On the second visit, after the examinations were performed, the patient returned to the outpatient clinic for an anthropometric assessment, which included measuring weight, height, Waist Circumference (WC) and BMI calculation and to receive nutritional recommendations to be followed. , in a qualitative way (characterized by the removal of foods with high fat content (fried preparations and with apparent fat), red meat, sugars in general, industrialized and increase of regulating foods, (sources of fiber, mainly soluble and water) and the 90 sachets, packed in brown envelopes, after being separated and identified with randomization, to start on the same day they received, considered as supplementation day 1. During the 90 days, patients were monitored by telephone, twice per week to check the quantity of available sachets.
The reassessment, called the third visit, took place on the first day of outpatient care after completion of supplementation, when patients were reassessed regarding anthropometric measurements (weight and WC) and IAQ (to verify adherence to dietary guidelines and referred to repeat the laboratory tests the day after the consultation.
The fourth visit was carried out 15 days after the exams were performed, when the new results were already available, to present the results to the patients.
The primary outcome measure consisted of a mean weight reduction of 500g per week. The secondary outcome consisted of the control of dysbiosis, lipid and glycemic profile.
Statistical analysis was performed according to intention to treat. The variables were described using absolute and relative frequencies (%) for the categorical and median and interquartile range to express the behavior of those of a quantitative nature, since the variables did not show a normal distribution. Afterwards, to verify the association of the results of the DIS questionnaire with those obtained from the INDICAN, the fisher's exact test was used. To compare the clinical and anthropometric variables between the groups, the non-parametric Mann Whitney test was used.
Data were analyzed using the IBM SPSS Statistics program, version 22.0.
Results
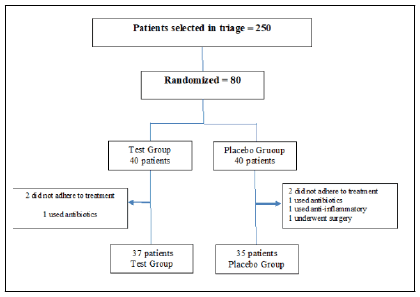
Of the 80 patients included according to the pre-established criteria, 72 completed the intervention period, 37 from the GT and 35 from the GP. Three patients from the GT and five from the GP left the study (Figure 1).
Table 1 presents some of the general characteristics of the patients studied. It is noteworthy that no significant differences were found between the two groups in relation to the variables, characterizing intergroup homogeneity (Table 1).
| Variables | Test (n = 37) | Placebo (n = 35) | P-Value |
|---|---|---|---|
| Age (years) | 53 ± 12 | 56 ± 13 | 0,72 |
| Average family income (R$) | 800,00 ± 120,00 | 720,00 ± 115,00 | 0,53 |
| BMI (kg/ m2) | 35,9 ± 6,5 | 34,5 ± 5,8 | 0,13 |
| Variables | Test (n = 37) | Placebo (n = 35) | P-Value |
| Weight | 98 [83.9:103.1] | 96.6 [87: 107] | 0.98 |
| WC | 105 [98:116] | 108 [101: 117] | 0.65 |
| Fasting glucose | 93.7 [90.8:101.1] | 95.6 [89:119] | 0.56 |
| Glycated hemoglobin | 6 [5.6:6.5] | 6.1 [5.7:7.1] | 0.75 |
| TC | 198 [171: 215] | 183 [147:208] | 0.45 |
| LDL | 123.05 [92.05: 135.7] | 110.2 [80.4:135.10] | 0.43 |
| HDL | 46.2 [42:56.1] | 43 [39.6:47.7] | 0.41 |
| TG | 134 [98:164.5] | 134 [86:180] | 0.2 |
| HOMA-IR Index | 3,81 [2,45:6,39] | 3,97 [2,02:7,23] | 0,15 |
Table 1: Baseline general characteristics of the groups.
Regarding education, 69% reported having completed high school and performing unpaid domestic activities; 99% declared themselves to be black. All reported unsuccessful weight loss attempts for more than five years. No difference was observed between the groups regarding weight and waist circumference.
Regarding the eating habits identified through the IAQ, it was found that 68.5% consumed large amounts of energy foods, rich in carbohydrates and lipids (including fried foods and red meat) in addition to having low intake of regulatory foods and water; 21.5% consumed regulating foods (rich in fiber), despite maintaining energy foods in their daily diet and 10% reported not consuming excess carbohydrates and fats. All consumed red meat at least 02 times a week. Regarding physical activity, 35% walked two to three times a week and 65% were sedentary. The evaluation of the DIS results showed that more than half (59.46%) of those who were part of the test group had medium risk, while for the GP this percentage was 45.71%. Added to this data are the results of the INDICAN parameter, as approximately 37% of the patients in both groups had dysbiosis (regardless of the classification) at the first moment of the evaluation.
Table 2 presents a comparison of anthropometric data between groups before and after the intervention. There was no absolute difference between the mean weights at the end of the study, but the analysis of the test group before and after treatment shows a median loss of 4.3% of body weight, with the difference in weight before and after the intervention statistically significant, while in the placebo group there was weight gain, without statistical significance (Table 2 & 3). No change in waist circumference was observed, but it was noted that the median of the GT was slightly smaller than the median of the GP both at the beginning and at the end of the study.
| Variable | Start (M1)* | P-value Mann Whitney Test | After 3 months (M2)** | P-Value Mann Whitney Test | ||
|---|---|---|---|---|---|---|
| Test | Placebo | Test | Placebo | |||
| Median (IIQ) | Median (IIQ) | Median (IIQ) | Median (IIQ) | |||
| Weight | 98 [83.9:103.1] | 96.6 [87: 107] | 0,12 | 93.8 [82.9:104] | 97 [85.1:106.9] | 0,65 |
| WC | 105 [98:116] | 108 [101:117] | 0,82 | 104.85 [100:115] | 105 [101:116] | 0,79 |
Table 2: Anthropometric assessment before and after the intervention-Intergroups. *Moment 1 and **Moment 2.
| Variable | Test Group | P-Value paired Wilcoxon | Placebo Group | P-Value paired Wilcoxon | ||
|---|---|---|---|---|---|---|
| Start | After 3 months | Start | After 3 months | |||
| Median (IIQ) | Median (IIQ) | Median (IIQ) | Median (IIQ) | |||
| Weight | 98 (83.9; 103.1) | 93.8 (82.9: 104) | 0,02 | 96.6 (87: 107) | 97 (85.1: 106.9) | 0,15 |
| WC | 105 (98; 116) | 104.85 (100: 115) | 0,11 | 108 (101: 117) | 105 (101: 116) | 0,09 |
Table 3: Anthropometric assessment before and after the intervention-Intragroups.
After providing guidance on food choices, there was a balance in relation to the adherence or not of patients between the groups, as 40% of the GT fully adhered against 37.84% of the GP. At the end of the study, 100% of the patients had a normal INDICAN. The analysis of the fecal pH results showed that both groups had a better profile (acid pH) after the intervention, as shown in Graphs 1 and 2, highlighting the best performance for the PG, however, without statistical significance.
Table 4 presents the laboratory parameters before and after the intervention in each group. The HOMA-IR index was high at the beginning of treatment in both groups, showing a high prevalence of insulin resistance, with no change observed after the intervention (Table 4). There was also no reduction in blood glucose or HbA1c. As for the lipid profile, it was possible to observe a reduction in LDL and an increase in HDL after the intervention in both groups, but with significance only in the placebo group.
| Variable | Test | Placebo | ||||
|---|---|---|---|---|---|---|
| Start | After 3 months | P-Value paired Wilcoxon | Start | After 3 months | P-value paired Wilcoxon | |
| Median (IIQ) | median (IIQ) | Median (IIQ) | Median (IIQ) | |||
| Fasting glucose | 93.7 (90.8:101.1) | 94.4 [87.3:117.3] | 0,35 | 95.6 [89:119] | 99.7 [89.2:129.3] | 0,88 |
| Glycated hemoglobin | 6 (5.6:6.5) | 6.2 [5.7:6.7] | 0,01 | 6.1 [5.7:7.1] | 6.3 [5.8:6.9] | 0,03 |
| TC | 198 (171:215) | 190 [170:203] | 0,15 | 183 [147:208] | 170 [142:197] | 0,06 |
| LDL | 123.05 (92.05:135.7) | 113 [90:131] | 0,11 | 110.2 [80.4:135.10] | 95 [75:121] | 0,02 |
| HDL | 46.2 (42:56.1) | 47 [41: 58] | 0,24 | 43 [39.6:47.7] | 46 [40:54] | 0,02 |
| TG | 134 (98:164.5) | 123 [100:155] | 0,20 | 134 [86:180] | 131 [81:173] | 0,81 |
| HOMA-IR Index | 3,81 [2,45:6,39] | 4,37 [2,395:6,095] | 0,12 | 3,97 [2,02:7,23] | 3,74 [2,09:7,56] | 0,26 |
Table 4: Metabolic assessment before and after intra-group intervention.
Discussion
It was observed in the present study that the sum of total and partial adherence by the patients to the nutritional guidelines provided was 57.14% and 54.06%, for the GT and GP, respectively, which represents a change in eating habits with the inclusion of foods with higher fiber content, especially soluble ones such as inulin and Fructooligosaccharides (FOS), which exert prebiotic action: They are not digestible, are fermentable by beneficial bacteria in the colon and can change the composition of the microbiota to a healthier type [24]. The aforementioned adherence to a diet with higher fiber content may explain the absence of dysbiosis and the better results of fecal pH in both groups after the intervention. Studies describe the effect of dietary fiber interventions on the composition of the intestinal microbiota in healthy adults, resulting in greater abundance of Bifidobacterium spp. and Lactobacillus spp., as well as higher fecal levels of butyrate production compared to the low fiber counter group [25,26]. As the two groups showed similar results, it is assumed that in the present study the effect of the diet, and not the probiotic, was effective in controlling dysbiosis and fecal pH.
Fruits, vegetables and whole grains are the main sources of fiber in the human diet [27]. They undergo microbial degradation and subsequent fermentation to the final AGCC products (butyrate, propionate and acetate). Butyrate produced mainly by Firmicutes [27] from the consumption of 30 g of soluble fiber, is the main source of energy for colonocytes and plays an important role in maintaining the intestinal barrier [28,29]. A diet low in fiber helps to reduce numerous specific bacterial rates and reduces diversity, contributing to the emergence and maintenance of dysbiosis. High animal fats such as meat and cheese dramatically and immediately changed the community structure of the gut microbiota in human participants in a short period of time (2 to 3 days) [30-32].
The main outcome investigated here was weight loss, identified, with a statistically significant difference in the Test Group. This result can be attributed to the use of the probiotic, since it was not found in the GP. The mean weight loss over the three months was 4.3% of body weight, close to the 5% considered successful intervention. Longer studies will be useful to better assess this effect.
The gut microbiota plays an important role in understanding the pathophysiology of obesity, which can be explained by the increased amounts of Firmicutes over Bacteroidetes, which result in methylation of genes related to obesity and other comorbidities in order to promote gene expression. And also to stimulate hormones that influence metabolic function by increasing the ability to capture energy. The intestinal microbiota influences the individual's metabolism, its ability to extract calories from food and its storage in adipose tissue, which predisposes an individual to obesity. Some mechanisms may explain this influence of the microbiota, such as the modulation of fat absorption and excretion, the reduction of endotoxemia and inflammation and the modulation of numerous genes involved in hepatic lipogenesis and/or adipose tissue lipolysis [33].
Other studies have revealed the importance of diet in the composition of the intestinal microbiota, genesis of obesity and the regulation of body weight. It has been observed that obese adults on a hypocaloric diet (both low-fat and low-carbohydrate) have increased fecal proportions of the phylum Bacteroidetes or subgroups of the genus Bacteroides, associated with weight loss and accompanied in some cases by reductions of the phylum Firmicutes or its subgroups. A lower proportion of Bacteroidetes and a higher proportion of Actinobacteria have also been associated with obesity, after comparing the fecal microbiota of obese and lean individuals [34].
Studies also show that the introduction of fibers can lead to a reduction in energy intake, which would lead to weight loss with consequent improvement in metabolic parameters [35]. This hypothesis could be verified by demonstrating that inulin supplementation was able to neutralize the effect of the increase in fat mass induced by the diet and in rats supplemented with resistant starch that showed lower weight gain and lower abdominal fat when compared to others that did not receive the same supplementation [36-38]. In this study, however, higher fiber consumption did not lead to weight loss as did the use of probiotics. There was also no significant difference between the groups regarding WC.
The analysis of the results of this research, referring to the lipid profile before and after the intervention with probiotics and the guidelines for a high-fiber diet, showed better results in both groups, but with no statistically significant difference between them, but significant in the placebo group before and after the intervention regarding LDL-c and HDL-c. It is important to highlight the hypolipidemic effect of fibers. Studies have led to the hypothesis that FOS could reduce hepatic lipogenic capacity by inhibiting gene expression of lipogenic enzymes, resulting in reduced secretion of VLDL-c. This inhibition could be achieved via SCFA production or via insulinemia modulation, through unknown mechanisms [39]. Reduction of TC and LDL-c was observed in obese patients after intervention with the use of fibers [40]. Although the insulinemia modulation pathway has already been described by studies through the use of fibers and also probiotics, in this study a better intra- and inter-group glycemic profile was not observed, despite specific cases having been identified.
As there was no significant difference in metabolic control between the groups at the two moments, the results found here contradict what most publications say regarding the impact of the use of probiotics aimed at controlling variables with a view to the secondary outcome. However, other studies have also failed to prove the benefits of using probiotics in isolation in humans [41].
The fact that the profile of the microbiota of the patients has not been defined, before and after the intervention, can be considered as a bias, in order to verify the types of predominant strains with a view to the F:B ratio, since it is known that specific intestinal bacteria and its metabolites affect host metabolism and feeding behavior and dysbiosis of this bio system can lead to metabolic syndrome [42]. In addition, other confounding factors that are difficult to control in research with humans can also be mentioned as influencing the results described here: the frequency of physical activity, the exact composition of the diet throughout the period (as this depends on the patients' acquisition), genetics, hormonal changes, the circadian cycle and hours of sleep, which should be considered in studies like this.
Conclusion
The results of this study suggest a beneficial effect of the use of probiotics with multiple strains associated with a diet rich in fiber with prebiotic action and reduced in sugars and fats in weight control, as well as demonstrating a positive effect of this same diet per se without the association of probiotics in the weight control, dysbiosis control and better lipid profile; however, as described, and contrary to other publications, neither probiotics nor dietary fibers alone were able to contribute to the control of the glycemic profile.
Thus, it is suggested that there is a need for further studies that aim to compare the effectiveness of the use of probiotics with or without prebiotics in controlling the variables investigated here, aiming to contribute with evidence that is sufficient to recommend the treatment of intestinal dysbiosis, controlling the possible biases identified here.
Funding
This study did not receive financial support.
Interest Conflicts
The authors declare that there are no conflicting interests.
All authors declare that the material has not been published elsewhere, or has not been submitted to another editor.
Data Availability
The authors declare that all related data are available from the corresponding author.
Acknowledgments
None.
References
- Magne F, Gotteland M, Gauthier L, et al. (2020) The firmicutes/bacteroidetes ratio: A relevant marker of gut dysbiosis in obese patients? Nutrients 12: 1474.
[Crossref], [Google Scholar], [Indexed]
- Cardinelli CS, Sala PC, Alves CC, et al. (2015) Influence of intestinal microbiota on bodyweight gain. A narrative review of the literature. Obes Surg 25: 346-353.
[Crossref], [Google Scholar], [Indexed]
- Cani PD, Amar J, Iglesias MA, et al. (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56: 1761-1772.
[Crossref], [Google Scholar], [Indexed]
- Amabebe E, Robert FO, Agbalalah T, Orubu ESF (2020) Microbial dysbiosis-induced obesity: Role of gut microbiota in homoeostasis of energy metabolismo. British Journal of Nutrition 123: 1127–1137.
[Crossref], [Google Scholar], [Indexed]
- Jandhyala SM, Talukdar R, Subramanyam C, et al. (2015) Role of the normal gut microbiota. World J Gastroenterol 21: 8787–8803.
[Crossref], [Google Scholar], [Indexed]
- Yong VB (2017) The role of the microbiome in human health and disease. An Introduction for Clinicians. BMJ 356.
[Crossref], [Google Scholar], [Indexed]
- Qin J, Li R, Raes J, et al. (2010) A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464: 59–65.
[Crossref], [Google Scholar], [Indexed]
- Dreyer JL, Liebl AL (2018) Early colonization of the gut microbiome and its relationship with obesity. Hum Microbiome J 10: 1-5.
[Crossref], [Google Scholar]
- Chakraborti CK (2015) New-found link between microbiota and obesity. World J Gastrointest Pathophysiol 6: 110–119.
[Crossref], [Google Scholar], [Indexed]
- Ley RE, Bäckhed F, Turnbaugh P, et al. (2005) Obesity alters gut microbial ecology. Proc Natl Acad Sci USA 102: 11070–11075.
[Crossref], [Google Scholar], [Indexed]
- Jumpertz R, Le DS, Turnbaugh PJ, et al. (2011) Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am J Clin Nutr 94: 58–65.
[Crossref], [Google Scholar], [Indexed]
- Turnbaugh PJ, Ley RE, Mahowald MA, et al. (2006) An obesityassociated gut microbiome with increased capacity for energy harvest. Nature 444: 1027–1031.
[Crossref], [Google Scholar], [Indexed]
- Davis CD (2016) The gut microbiome and its role in obesity. Nutr Today 51: 167–174.
[Crossref], [Google Scholar], [Indexed]
- Hu H-J, Park S-G, Jang HB, et al. (2015) Obesity alters the microbial community profile in Korean adolescents. Plos One 10: e0134333.
[Crossref], [Google Scholar], [Indexed]
- Schwiertz A, Taras D, Schäfer K, et al. (2010) Microbiota and SCFA in lean and overweight healthy subjects. Obesity 18: 190–195.
[Crossref], [Google Scholar], [Indexed]
- Robson, A (2009) Preventing diet-induce disease: Bioavailable diets rich in nutrientes and low energy. Nutrition and Health 20(2): 135-166.
[Crossref], [Google Scholar], [Indexed]
- Ghoorah K, Campbell P, Kent A, et al. (2016) Obesity and cardiovascular results: A review. European Heart Journal: Acute Cardiovascular Care 5(1): 77-85.
[Crossref], [Google Scholar]
- Roberfroid M, Gibson GR, Hoyles L, et al. (2010) Prebiotic effects: Metabolic and health benefits. Br J Nutr 104: S1–S63.
[Crossref], [Google Scholar], [Indexed]
- Lim CC, Ferguson LR, Tannock GW (2005) Dietary fibres as "prebiotics": Implications for colorectal cancer. Mol Nutr Food Res 49: 609–619.
[Crossref], [Google Scholar], [Indexed]
- OMS (1997) In: Kappari I. guy's day medicine ambulatory a hospitaller. Unifesp/EPM, Nutricao 92.
- Diretrizes da Sociedade Brasileira de Diabetes 2017-2018. Organized by Jose Egidio Paulo de Oliveira, Renan Magalhaes Montenegro Junior, Sergio Vencio. Clannad. 2017.
- Stern M, Kahn R, Buse J, Ferrsnnini E (2005) The metabolic syndrome: Time for a critical appraisal: Joint statement from the American diabetes association and the European association for the study of diabetes. Diabetes Care 28(9): 2289–2304.
[Crossref], [Google Scholar], [Indexed]
- https://www.infopedia.pt/dicionarios/termos-medicos/reacao de Obermayer.
- Petschow B, Dore J, Hibberd P, et al. (2013) Probiotics, prebiotics, and the host microbiome: The science of translation. Ann N Y Acad Sci 1306(1): 1-17.
[Crossref], [Google Scholar], [Indexed]
- Diamant M, Blaak EE, Vos WM (2011) Do nutrient-gutmicrobiota interactions play a role in human obesity, insulin resistance and type 2 diabetes? Obes Rev 12(4): 272-81.
[Crossref], [Google Scholar], [Indexed]
- So D, Whelan K, Rossi M, et al. (2018) Dietary fiber intervention in the composition of the intestinal microbiota in healthy adults: A systematic review and meta-analysis. J Clin Nutr 107: 965–983.
[Crossref], [Google Scholar], [Indexed]
- Moszak M, SzuliNska M, BogdaNski P (2020) You are what you eat-the relationship between diet, microbiota, and metabolic disorders-A Review. Nutrients 12: 1096.
[Crossref], [Google Scholar], [Indexed]
- Mills S, Stanton C, Lane JA, et al. (2019) Precision nutrition and microbiome, part I: Current state of science. Nutrients 11: 923.
[Crossref], [Google Scholar], [Indexed]
- Parada Venegas D, De la Fuente MK, Landskron G, et al. (2019) Short Chain Fatty Acids (SCFAs)-mediated gut epithelial and Immune Regulation and its relevance for inflammatory bowel diseases. Front Immunol 10: 1486.
[Crossref], [Google Scholar], [Indexed]
- Scott KP, Duncan SH, Flint HJ (2008) Dietary fiber and intestinal microbiota. Nutr Touro 33: 201-211.
[Crossref], [Google Scholar]
- David LA, Maurice CF, Carmody RN, et al. (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature.
[Crossref], [Google Scholar], [Indexed]
- Carmody RN, Gerber GK, Luevano JM, et al. (2015) Diet dominates host genotype in shaping the murine gut microbiota. Cell Host Microbe.
[Crossref], [Google Scholar], [Indexed]
- Prados-Bo A, et al. (2015) El papel de los probióticos en el manejo de la obesidade. Nutr Hosp 31(S1): 10-18.
[Crossref], [Google Scholar], [Indexed]
- Sanz Y, Rastmanesh R, Agostoni C (2013) Understanding the role of gut microbes and probiotics in obesity: how far are we? Pharmacol Res 69(1): 144-155.
[Crossref], [Google Scholar], [Indexed]
- Wang L, Li P, Tang Z, Yan X, Feng B (2016) Structural modulation of the gut microbiota and the relationship with body weight: compared evaluation of liraglutide and saxagliptin treatment. Sci Rep.
[Crossref], [Google Scholar], [Indexed]
- Frota KGM, et al. (2015) Effect of prebiotics and probiotics on intestinal microbiota and metabolic changes in obese individuals. Nutrire 40(2): 173-187. [Crossref], [Google Scholar], [Indexed]
- Dewulf EM, Cani PD, Neyrinck AM, et al. (2011) Inulin-type fructans with prebiotic properties counteract GPR43 overexpression and PPARÃŽ³-related adipogenesis in the white adipose tissue of high-fat diet-fed mice. J Nutr Biochem 22(8): 712-22.
[Crossref], [Google Scholar], [Indexed]
- Keenan MJ, Janes M, Robert J, et al. (2013) Resistant starch from high amylose maize (HAM-RS2) reduces body fat and increases gut bacteria in ovariectomized (OVX) rats. Obesity 21 (5): 981-4.
[Crossref], [Google Scholar], [Indexed]
- Delzenne NM, Daubioul C, Neyrinck A, et al. (2002) Inulin and oligofructose modulate lipid metabolism in animals: review of biochemical events and future prospects. Br J Nutr Wallingford 87: 255-259.
[Crossref], [Google Scholar], [Indexed]
- David LA, Maurice CF, Carmody RN, et al. (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature 505: 559–563.
[Crossref], [Google Scholar], [Indexed]
- Raoult D (2008) Obesity pandemics and the modification of digestive bacterial flora. Eur J Clin Microbiol Infect Dis 27: 631–634.
[Crossref], [Google Scholar], [Indexed]
- Yacyshyn PLMR, Yacyshyn B (2019) Gut microbiota and obesity: An opportunity to alter obesity through faecal microbiota transplant (FMT). Diabetes, Obesity and Metabolism 1(3).
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences